by William Clearfield, D.O. for Longevinex
“A little-discussed yet vital aspect of overall well-being is the interplay between hormone sufficiency and brain health. Today, we delve into the profound effects of testosterone, estrone, estradiol, progesterone, thyroid hormones, cortisol, insulin, growth hormone, DHEA, pregnenolone, and prolactin on the brain’s intricate functions. We explore how maintaining optimal hormonal balance serves as a potent safeguard against cognitive decline, dementia, and the devastating progression of Alzheimer’s disease. By shedding light on this crucial topic, we aim to empower our readers with the knowledge necessary to foster a healthier, more vibrant mind throughout the various stages of life.”
Introduction
Do you recall our comprehensive ten-step program aimed at enhancing brain health? It’s a pivotal guide for maintaining cognitive vitality, especially as we age. Let’s briefly revisit the steps:
- Step 1: Maintain balanced blood sugar levels.
- Step 2: Incorporate healthy fats into your diet.
- Step 3: Prioritize adequate and restorative sleep.
- Step 4: Ensure optimal Vitamin D3 intake for brain function.
- Step 5: Focus on gut health.
- Step 6: Ensure proper methylation processes.
- Step 7: Keep your hormones in equilibrium.
- Step 8: Implement six key strategies for heart health.
- Step 9: Stay active with regular exercise.
- Step 10: Embrace lifelong learning.
We’re here to pick up where we left off, delving into Step 7 with the same dedication to supporting your brain health. Join us as Longevinex continues this vital conversation, ensuring your cognitive well-being remains a top priority.
Hormone Optimization to Boost Brain Health
Hormones, our body’s chemical messengers, carry instructions from their organ of origin to receptor cells in end organs. Hormones regulate, among other things, hunger, emotions, energy balance, equilibrium, sexual energy and function, hair growth, and brain health. In short, hormones, the “juice of life,” control our quality of life. A body deprived of hormones, think menopause, or in men “andropause,” is akin to the caterer not showing up at your wedding reception. You can make it work, but the afterparty will hardly be what you dreamed of for your special day. (2)
Hormones have a terrible reputation. Poorly understood and utilized incorrectly for decades, when one thinks of hormones, our knee-jerk reaction is, “Hormone! Oh no. Not for me. Hormones = cancer.”
And to a degree, that’s true. Certain hormones, specifically manufactured synthetic hormones derived from horse urine, are altered to make them unique and patentable and contain as little as 30% human genetic material. (3)
Natural, chemically identical to our hormones, are, at worst, neutral regarding cancer development and, for the most part, protect against neoplasms. (4-5)
Commonly associated with libido, sexual energy, and function, hormones are nature’s genuine antiaging substances. In men, hormone sufficiency leads to enhanced energy and muscle tone, improved exercise endurance, effective fat loss, better sleep, regrowth of scalp hair, reduced joint pain and muscle aches, stronger bones, improved lipid levels, heart disease protection, and sharpened memory and concentration. (6)
In women, hormone adequacy results in improved energy, fat loss acceleration, muscle tone, sex drive, bone strength, wrinkle reduction, mood elevation, memory, and concentration. (7)
The risk of heart disease in women with adequate hormone levels beyond menopause is reduced by up to 50 %. Night sweats, hot flashes, vaginal dryness, itching, and painful intercourse all disappear when hormones are balanced.
Unfortunately, these chemicals, the hormones that keep us youthful, lush, and full of vigor, begin to peter out around age 25-27. Otherwise, life expectancy, which for the most part has advanced steadily over the past 100 years with modern medical miracles and hormone optimization, would be what it is in places like Nigeria today, 53 years old. (8)
The effects of hormone depletion on the human body are universal. Our skin shrivels, our hair turns white if it doesn’t fall out altogether, our fingernails crack and break, our bones soften, and our organs fail. Hormone optimization softens the “fall” a soft landing, allowing us to mature with ease and grace.
A little-discussed aspect of optimal hormone health revolves around hormonal influences on brain health. Today, we present a deep dive into the effects of testosterone, estrone, estradiol, progesterone, the thyroid hormone, cortisol, insulin, growth hormone, DHEA, pregnenolone, and prolactin on the brain. We accept bonus pats on the back for discussing the critical role of hormone optimization in preventing cognitive decline, dementia, and Alzheimer’s disease.
A little-discussed yet vital aspect of overall well-being is the interplay between hormone sufficiency and brain health. Today, we delve into the profound effects of testosterone, estrone, estradiol, progesterone, thyroid hormones, cortisol, insulin, growth hormone, DHEA, pregnenolone, and prolactin on the brain’s intricate functions. We explore how maintaining optimal hormonal balance serves as a potent safeguard against cognitive decline, dementia, and the devastating progression of Alzheimer’s disease. By shedding light on this crucial topic, we aim to empower our readers with the knowledge necessary to foster a healthier, more vibrant mind throughout the various stages of life.
—
Testosterone
Beyond its role in male sexual health, testosterone supports brain health. Adequate testosterone reserves provide relief from anxiety and depression and improve one’s sense of well-being. Testosterone enhances cognitive abilities, memory, and concentration while preventing neurodegenerative diseases. (9)
—
Estrone
The weakest of the three types of estrogen, the others being estradiol, the “female characteristics” hormone, and estriol, the “pelvic health” hormone, estrone metabolizes down the cancer-causing pathways. With the aid of 7 keto DHEA, our goal is to keep estrone less than 100 pg/mL. In terms of brain health, estrone impacts memory retention and processing. Excess estrone manifests with mood swings and insomnia. (10)
Estradiol
Estradiol, the most potent of the three forms of estrogen, dilates small blood vessels, thus providing essential nutrients for learning and memory, and drives blood flow to the brain. Estradiol levels in the upper third of its reference range correlate with better cognitive function and aid in forming the neurotransmitter serotonin. Serotonin, in turn, decreases depression, irritability, anxiety, and pain sensation. (11)
Progesterone
Progesterone, the most prominent hormone in the second half of the menstrual cycle, is a neuroprotectant that preserves and directs brain tissue repair after injury. Progesterone balances estrogen and stimulates GABA production. GABA is the calming neurotransmitter providing relief from mood and emotional upheaval.
Low progesterone presents as agitation, irritability, insomnia, low libido, headaches, mood swings, memory loss, brain fog, and a short temper. Low progesterone behaviors include anxiety, sadness, and depression. (12)
—
Thyroid Hormone
The thyroid hormones are your “gas pedal.” The thyroid provides the fuel critical for metabolic function and, not surprisingly, significantly influences the brain. When functioning properly, adequate “fuel,” i.e., thyroid hormones, are necessary for brain maturation in the developing fetus and memory and attention in adult men and women. Thyroid hormone optimization improves cognitive function.
10-30% of all traumatic brain injury patients develop new-onset hypothyroidism three months to seventeen years post-injury. The brain produces neurochemicals, serotonin, dopamine, glutamate, and GABA, to perform its myriad functions. The thyroid acts as a fine-tuning mechanism to ensure the smooth transmission of these messengers to the rest of the body. When thyroid function is suppressed, as in TBI, cognitive performance declines. (13)
—
Cortisol
Cortisol, the “fight or flight” hormone, is the body’s first line of defense. Produced in the adrenal glands, cortisol is always at the ready to respond to insults to our well-being, great and small.
When last we fended off the pterodactyl, rounding behind the giant rock at the end of the universe, only to be confronted by a mountain lion looking for its next meal behind the next rock, we felt a rush (of adrenaline), produced by cortisol, to provide us with the energy and means to fight back. Once we arm wrestled the mountain lion out of the way, Fred Flintstone style, and the danger passed, our cortisol drops to its sub-noticeable “calm” state until the next crisis. Next, when T Rex shows his ugly head, the cycle repeats.
At least, that’s how the system is supposed to work. In the real world, with most of us busily putting out fire after fire day and night, we constantly call on our cortisol reserve to bail us out of trouble. But we can only make so much. The constant “high” we experience with excess cortisol in our system eventually burns itself out, leading to a condition known 100 years ago as neurasthenia. Today, we call it adrenal fatigue. Without proper rest, relaxation, and renewal, our body is at first overrun with excess, then insufficient cortisol to protect our being.
The results of chronic cortisol overload include excessive morning fatigue with a need for mid-morning stimulation; caffeine comes to mind. By mid-afternoon, we need a nap. By 6 PM, we are thoroughly exhausted. Later at night, eight, nine, and ten o’clock, we experience an awakening. This late-night awakening is when we do our best work and are most alert. Then, we have trouble falling asleep as we are “wound up,” Accompanying this late-night energy surge is associated with sugar and salt cravings. (14)
Elevated cortisol levels decrease the size of specific brain structures, most notably the hippocampus. Hippocampal atrophy leads to impaired cognitive abilities and memory.
Chronically elevated cortisol levels impact dopamine production, leading to the blockade of prolactin-inhibiting factors, causing a semipermanent rise in cortisol with resultant “treatment-resistant” anxiety and panic attacks. (15)
—
Insulin
Well-known for its role in glucose metabolism, insulin is neuroprotective. Insulin influences cerebral function by regulating brain glucose metabolism. Insulin resistance, when cells in our muscles, fat, and liver don’t respond as they should to insulin, is associated with diminished cognitive performance and an increased risk of neurodegenerative diseases. (16)
—
Growth Hormone
Growth Hormone (GH) plays a crucial role in physical growth, cognitive development, and brain health. GH stimulates the formation of new neurons while protecting senescent cells from death. Adult onset Growth Hormone deficiency reduces memory and cognitive function. (17)
Symptoms of Adult Growth Hormone deficiency include gaps in memory, concentration, the ability to start and finish projects, and multitasking. This loss, termed “Executive Function,” includes obsessive-compulsive tendencies, dark moods, and paranoias. (18)
Growth Hormone replacement therapy reverses these symptoms while preventing cognitive decline due to aging. (19)
—
DHEA
Dehydroepiandrosterone (DHEA) is a precursor to estrogen and testosterone. It is linked to cognitive performance while enhancing brain health. (20)
DHEA and cortisol are important cofactors in regulating physical maturation and brain development. High DHEA levels are associated with neuroprotection, while high cortisol levels lead to catabolic and neurologic destruction. DHEA offsets cortisol, providing acriticaly insight into reversing the toxic effects of elevated cortisol. (21)
Optimal DHEA to cortisol (D/C) ratios measure at 4-7/1. Elevated D/C ratios indicate favorable cognitive ability up to a point. Very high D/C ratios manifest as panic disorders, while Low D/C ratios develop into the catabolic states of chronic stress, hypothalamic-pituitary-adrenal imbalance, cognitive and mood disorders, anxiety, and depression (22).
—
Pregnenolone
Pregnenolone is the hormone of memory, mood, and neuroprotection. (23)
In our practice, we measure pregnenolone levels in every patient. This metric gives us insights into where our patients are cognition-wise during the examination. We administer pregnenolone for memory disorders, further underlining its importance in cognitive function. (24)
—
Prolactin
Best known for its role in lactation, prolactin influences emotional and cognitive processes and impacts neurogenesis and myelination. Prolactin aids in treating demyelinating diseases, such as multiple sclerosis, highlighting its diverse role in brain function. (25)
—
Summary
Balancing the ten major hormones—testosterone, estrone, estradiol, progesterone, the thyroid hormones, cortisol, Insulin, growth hormone, DHEA, pregnenolone, and prolactin—is crucial for optimal brain health. Each messenger “chemical” uniquely contributes to cognitive function, mood regulation, and neuroprotection.
Approaching aging and wellness through a ‘hormone-centric’ lens is a significant leap forward in evaluating and maintaining cognitive health. When balanced, hormones aid in the prevention of and management of cognitive decline, dementia, and Alzheimer’s disease.
Understanding and managing the intricacies of hormone optimization is a rewarding medical subspecialty. My colleagues and I, who study and practice this subspecialty, offer root-cause versus the usual “drug-covered” ways to diagnose and remedy cognitive decline and enhance overall brain health.
It is not easy, and there are no quick fixes. We advise our patients that it can take six months, a year, or even two years of intense therapy to yield results.
I want to leave you, our loyal readers, with this declaration: If I did not or could not practice this art of hormone optimization, I would be driving an Uber.
Dr. William Clearfield
March 2024
xxxxxx
—
References
- https://longevinex.com/articles/
- https://www.weddingwire.com/biz/revolve-pizza-kitchen/4e89525cd9dd20a4.html
- Klein, R., The Composition of Premarin. Int. J Fertility 43:223 1998
- Fournier, A., et al., “Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study,” Breast Cancer Res Treat 2008; 107(1):103-11.
- Dimitrakakis C, Jones RA, Liu A, Bondy CA. Breast cancer incidence in postmenopausal women using testosterone in addition to usual hormone therapy. Menopause. 2004 Sep-Oct;11(5):531-535.
- Furrer R, Hawley JA, Handschin C. The molecular athlete: exercise physiology from mechanisms to medals. Physiol Rev. 2023 Jul 1;103(3):1693-1787. doi: 10.1152/physrev.00017.2022. Epub 2023 Jan 5. PMID: 36603158; PMCID: PMC10110736.
- Hodis HN, Mack WJ. Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It Is About Time and Timing. Cancer J. 2022 May-Jun 01;28(3):208-223. doi: 10.1097/PPO.0000000000000591. PMID: 35594469; PMCID: PMC9178928.
- https://bhrttrainingacademy.com/what-happens-when-women-age/
- Wahjoepramono EJ, Asih PR, Aniwiyanti V, Taddei K, Dhaliwal SS, Fuller SJ, Foster J, Carruthers M, Verdile G, Sohrabi HR, Martins RN. The Effects of Testosterone Supplementation on Cognitive Functioning in Older Men. CNS Neurol Disord Drug Targets. 2016;15(3):337-43. doi: 10.2174/1871527315666151110125704. PMID: 26553159; PMCID: PMC5078598.
- https://my.clevelandclinic.org/health/body/22398-estrone
- Xu Q, Ji M, Huang S, Guo W. Association between serum estradiol levels and cognitive function in older women: a cross-sectional analysis. Front Aging Neurosci. 2024 Feb 21;16:1356791. doi: 10.3389/fnagi.2024.1356791. PMID: 38450384; PMCID: PMC10915044.
- Berent-Spillson A, Briceno E, Pinsky A, Simmen A, Persad CC, Zubieta JK, Smith YR. Distinct cognitive effects of estrogen and progesterone in menopausal women. Psychoneuroendocrinology. 2015 Sep;59:25-36. doi: 10.1016/j.psyneuen.2015.04.020. Epub 2015 May 14. PMID: 26010861; PMCID: PMC4490102.
- Revisiting Thyroid Hormones in Schizophrenia. Journal of Thyroid Research Volume 2012, Article ID 569147. N. Santos, et. et al. e and Health Sciences Research Institute, School of Health Sciences, University of Minho, Campus de Gualtar, Braga, Portugal, Dept of Pathology, Leiden University Medical Center, Leiden, The Netherlands Institute of Medical Psychology, Faculty of Medicine, U. of Coimbra, Coimbra, Portugal
- Metcalf, Eric, http://www.webmd.com/a-to-z-guides/features/adrenal-fatigue-is-it-real, Accessed February 16, 2015
- Cognitive Functioning, Cortisol Release, and Symptom Severity in Patients with Schizophrenia. BIOL PSYCHIATRY 2000;48:1121–1132. Deborah J. Walder, Elaine F. Walker, and Richard J. Lewine. Departments of Psychology and Psychiatry, Emory University, Atlanta, Georgia.
- Ma, L., Wang, J., & Li, Y. (2015). Insulin resistance and cognitive dysfunction. Clinica Chimica Acta, 444, 18-23. https://doi.org/10.1016/j.cca.2015.01.027
- Tresguerres JÁF, Fernández-Tresguerres I, Viña J, Rancan L, Paredes SD, Linillos-Pradillo B, Vara E. Effects of GH on the Aging Process in Several Organs: Mechanisms of Action. Int J Mol Sci. 2022 Jul 16;23(14):7848. doi: 10.3390/ijms23147848. PMID: 35887196; PMCID: PMC9318627.
- Maruff P, Falleti M. Cognitive function in growth hormone deficiency and growth hormone replacement. Horm Res. 2005;64 Suppl 3:100-8. doi: 10.1159/000089325. Epub 2006 Jan 20. PMID: 16439852.
- Colon G, Saccon T, Schneider A, Cavalcante MB, Huffman DM, Berryman D, List E, Ikeno Y, Musi N, Bartke A, Kopchick J, Kirkland JL, Tchkonia T, Masternak MM. The enigmatic role of growth hormone in age-related diseases, cognition, and longevity. Geroscience. 2019 Dec;41(6):759-774. doi: 10.1007/s11357-019-00096-w. Epub 2019 Sep 4. PMID: 31485887; PMCID: PMC6925094.
- Marcello Maggio, E. Dall’Aglio, F. Lauretani, et al., The hormonal pathway to cognitive impairment in older men, The Journal of Nutrition, Health and Aging, Volume 16, Issue 1, 2012, Pages 40-54, ISSN 1279-7707, https://doi.org/10.1007/s12603-012-0002-7
- Whitham JC, Bryant JL, Miller LJ. Beyond Glucocorticoids: Integrating Dehydroepiandrosterone (DHEA) into Animal Welfare Research. Animals (Basel). 2020 Aug 9;10(8):1381. doi: 10.3390/ani10081381. PMID: 32784884; PMCID: PMC7459918.
- https://healthmatters.io/understand-blood-test-results/dhea-cortisol-ratio
- Ramírez S, Haddad-Tóvolli R, Radosevic M, Toledo M, Pané A, Alcolea D, Ribas V, Milà-Guasch M, Pozo M, Obri A, Eyre E, Gómez-Valadés AG, Chivite I, Van Eeckhout T, Zalachoras I, Altirriba J, Bauder C, Imbernón M, Garrabou G, Garcia-Ruiz C, Nogueiras R, Soto D, Gasull X, Sandi C, Brüning JC, Fortea J, Jiménez A, Fernández-Checa JC, Claret M. Hypothalamic pregnenolone mediates recognition memory in the context of metabolic disorders. Cell Metab. 2022 Feb 1;34(2):269-284.e9. doi: 10.1016/j.cmet.2021.12.023. PMID: 35108514; PMCID: PMC8815774.
- Ramírez S, Haddad-Tóvolli R, Radosevic M, Toledo M, Pané A, Alcolea D, Ribas V, Milà-Guasch M, Pozo M, Obri A, Eyre E, Gómez-Valadés AG, Chivite I, Van Eeckhout T, Zalachoras I, Altirriba J, Bauder C, Imbernón M, Garrabou G, Garcia-Ruiz C, Nogueiras R, Soto D, Gasull X, Sandi C, Brüning JC, Fortea J, Jiménez A, Fernández-Checa JC, Claret M. Hypothalamic pregnenolone mediates recognition memory in the context of metabolic disorders. Cell Metab. 2022 Feb 1;34(2):269-284.e9. doi: 10.1016/j.cmet.2021.12.023. PMID: 35108514; PMCID: PMC8815774.
- Paul DA, Rodrigue A, Contento N, Haber S, Hoang R, Rahmani R, Hirad A, Shafiq I, Williams Z, Vates GE. Prolactin at moderately increased levels confers a neuroprotective effect in non-secreting pituitary macroadenomas. PLoS One. 2022 Aug 3;17(8):e0271690. doi: 10.1371/journal.pone.0271690. PMID: 35921360; PMCID: PMC9348739.
Share
Introduction In a world where health is increasingly prioritized, the interplay of different body systems is more evident than ever. The link between heart health and brain function is crucial yet often overlooked. (1) For […]
Introduction The search for ways to live longer has led to the development of anti-aging supplements that aim to slow down the natural process of aging. Two such supplements that have gained attention are NMN […]
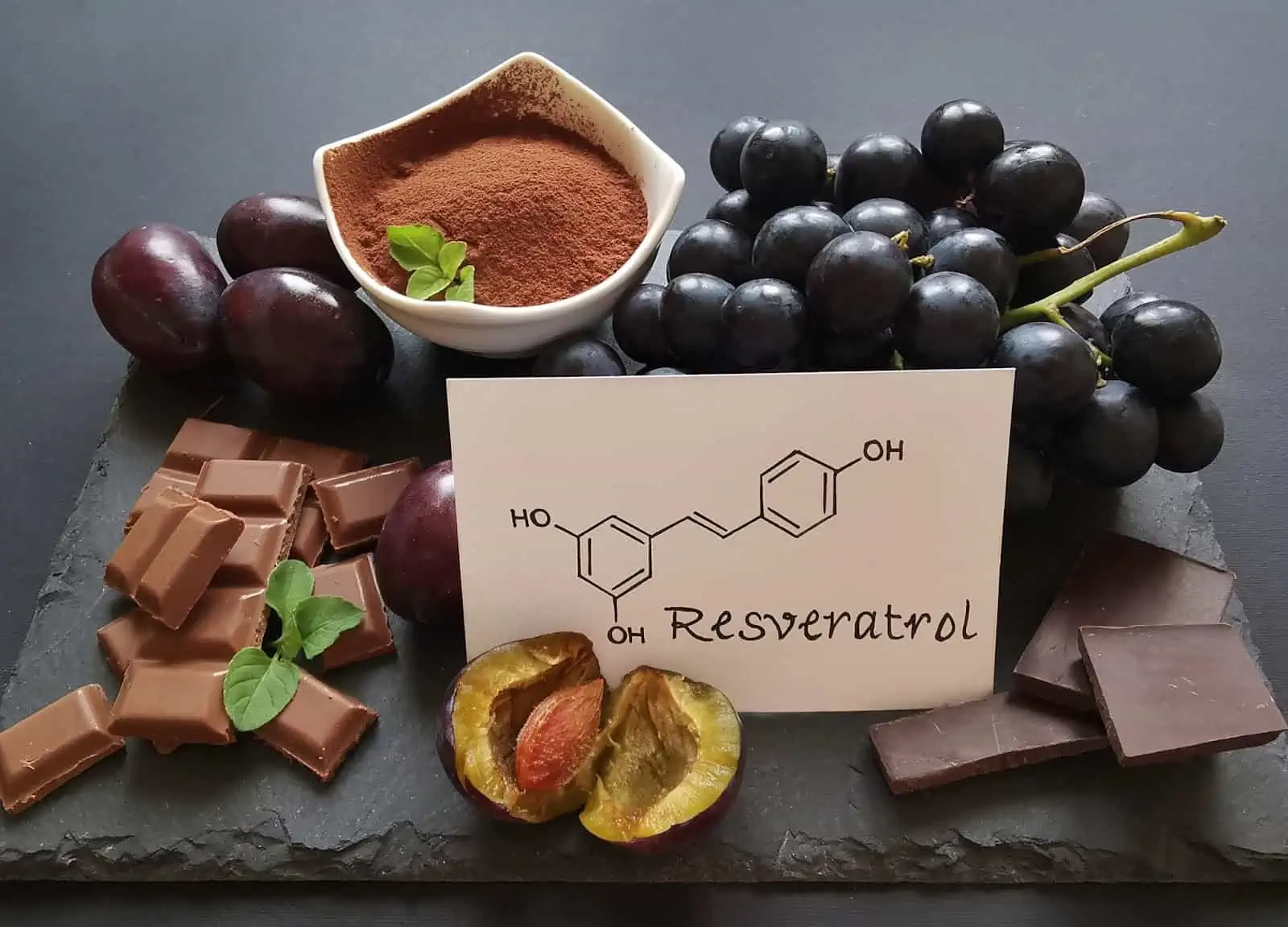
Introduction In today’s health-conscious society, resveratrol supplements are gaining increasing attention for their numerous health benefits. A naturally occurring compound mainly found in grape skins and red wine, resveratrol is praised for its antioxidant properties […]